Prescription Drug Misuse: Risks, Signs, and What to Do
When you take a pill because your doctor said so, it’s medicine. But when you take it differently—higher doses, more often, or just because it feels good—that’s prescription drug misuse, the improper use of medications prescribed for medical conditions. Also known as pharmaceutical abuse, it’s not always about street drugs. It’s often your own medicine, taken in ways it was never meant to be. This isn’t just about opioids. It’s about sleeping pills you pop to get through the week, painkillers you keep on hand "just in case," or ADHD meds you borrow to stay focused. The line between treatment and abuse is thinner than most people realize.
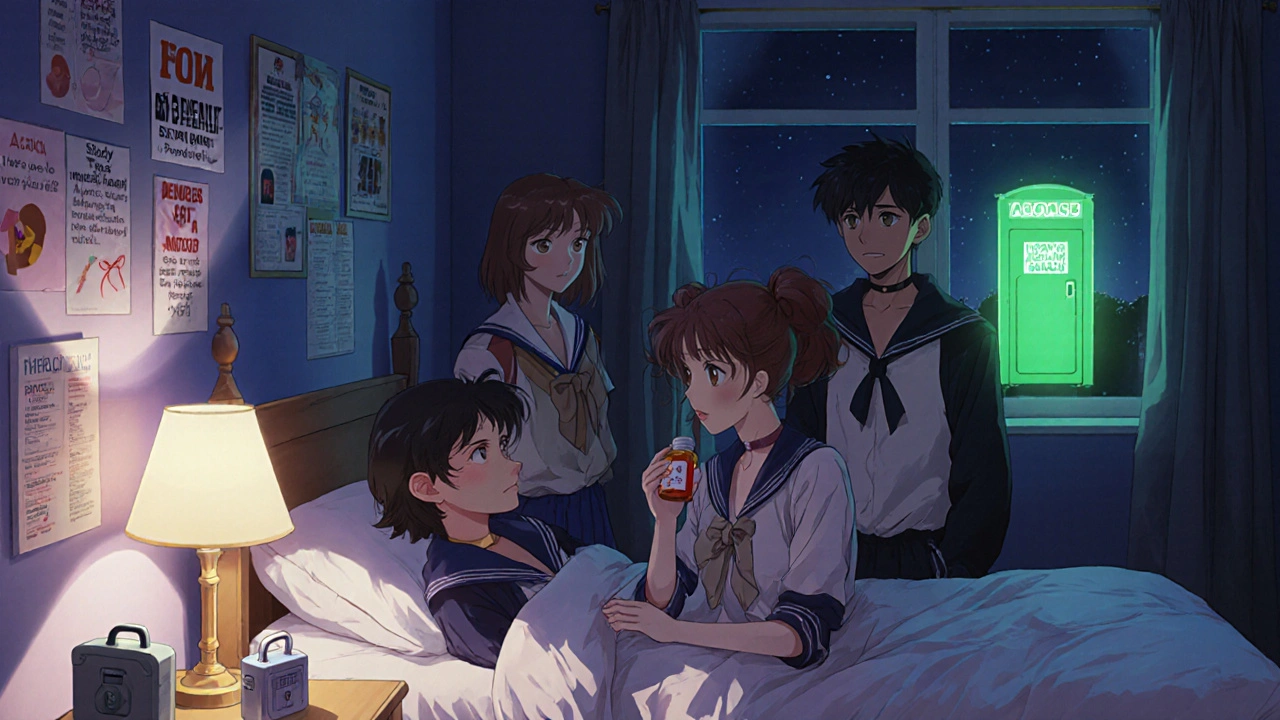
People don’t always start out trying to get high. Many begin with a legitimate need—chronic pain, anxiety, insomnia—and over time, the body changes. Tolerance builds. The original dose doesn’t work like it used to. Then comes the mental shift: "I need this to feel normal." That’s when drug dependence, a physical or psychological need for a substance to function kicks in. And when dependence meets access—like leftover pills from a past surgery or a friend’s extra prescription—it turns into opioid abuse, the misuse of pain medications like oxycodone, hydrocodone, or fentanyl. These drugs slow breathing. A little extra can stop it completely. That’s why mixing them with alcohol or benzodiazepines is deadly. Even harmless-seeming drugs like muscle relaxers or anti-anxiety meds can become dangerous when combined with other prescriptions, like the heart meds or blood thinners mentioned in our posts.
What makes this worse is how often it’s hidden. No one walks around saying, "I’m addicted to my Xanax." People say, "I just need it to sleep," or "My back hurts worse than before." The signs aren’t always obvious: mood swings, doctor shopping, hiding pills, skipping work, or sudden changes in sleep or appetite. And if you’re taking multiple medications—like statins, anticoagulants, or antidepressants—you’re already at higher risk for dangerous interactions. That’s why posts on warfarin and ibuprofen, paroxetine weight gain, or rifampin drug interactions matter. They’re not just about side effects. They’re about understanding how your body reacts when you use these drugs outside their intended path.
You don’t have to wait until things spiral to get help. Recognizing misuse early changes everything. This collection of articles doesn’t just list risks. It shows you what to look for, what to ask your doctor, and how to spot when a medication isn’t working the way it should. From how long withdrawal lasts after stopping antidepressants, to why the first generic filer gets 180 days of exclusivity (and how that affects drug availability), these posts connect the dots between policy, biology, and real-life choices. What you’ll find here isn’t fearmongering. It’s clarity. Real facts. Real stories. And real ways to protect yourself and others from the quiet crisis hiding in medicine cabinets across the country.