When you pick up a prescription, you might not realize you have the right to say no. Pharmacists often swap your brand-name medication for a cheaper generic version - sometimes without telling you. But you don’t have to accept it. In many states, you can legally refuse a generic substitution and ask for the brand-name drug instead. This isn’t about being picky. For some people, even small changes in medication can cause serious problems. Knowing your rights can protect your health.
What Is Generic Substitution?
Generic drugs are copies of brand-name medications. They contain the same active ingredient, work the same way, and are approved by the FDA as safe and effective. But they’re not identical. They may have different fillers, dyes, or coatings. For most people, this doesn’t matter. But for others - especially those taking drugs with a narrow therapeutic index (NTI) - these differences can change how the medicine works in the body.Drugs like levothyroxine (for thyroid issues), warfarin (a blood thinner), and certain epilepsy medications fall into this high-risk category. Even tiny shifts in dosage can lead to seizures, blood clots, or heart problems. The FDA calls these drugs "therapeutically equivalent," but doctors and patients know better. Many have seen what happens when a switch goes wrong.
Pharmacists are allowed to substitute generics by default in most states. But that doesn’t mean you have to accept it. You have the right to say no - and in some places, they can’t even make the switch without your permission.
Your Legal Right to Refuse
Laws vary by state. In 19 states, including California, Texas, and New York, pharmacists are required to substitute generics unless told otherwise. In 7 states - Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, and Vermont - plus Washington, D.C., they must get your explicit consent before switching. That means they can’t just hand you a different pill. They have to ask: "Do you want the generic?"In 31 states and D.C., pharmacists must notify you - verbally or in writing - that a substitution is happening. That gives you a chance to speak up. But in 24 states, there’s no legal protection if something goes wrong after a substitution. You’re left with little recourse.
The bottom line? You always have the right to refuse. Even in states where substitution is automatic, saying "I decline substitution" is enough. You don’t need a doctor’s note. You don’t need to explain why. Just say it clearly at the counter.
When You Should Ask for the Brand Name
Not everyone needs to fight for brand-name drugs. But if you’ve had issues before - side effects, unstable blood levels, or a bad reaction after switching - you’re not alone. Here’s when to speak up:- You take a narrow therapeutic index drug (like levothyroxine, digoxin, or phenytoin)
- You’ve been on the same brand for years and your condition is stable
- You’ve had side effects after switching generics in the past
- You’re on a biologic (like insulin, Humira, or Enbrel) - these aren’t true generics and can behave differently
- You’re on Medicaid, Medicare, or private insurance that has a history of forcing switches
Insulin users, for example, report wild blood sugar swings after being switched to biosimilar versions like Basaglar or Semglee. One patient on a diabetes forum said it took two weeks to realize the problem wasn’t his diet - it was the new insulin. He had to go back to Lantus to regain control.
Thyroid patients often feel fatigued, gain weight, or get heart palpitations after switching from Synthroid to a generic. Why? Because levothyroxine is absorbed differently depending on the filler. Even a 5% change can throw off your hormone levels. Your doctor may not know unless you tell them.
How to Actually Refuse a Generic
Saying "no" sounds simple. But pharmacists sometimes push back. They might say:- "It’s required by law."
- "You’ll pay more if you don’t switch."
- "We have to do this."
None of those are true in states that require consent. Here’s how to handle it:
- At the counter, say clearly: "I decline substitution. I want the brand-name drug as prescribed."
- If they argue, ask to speak with the manager. Pharmacists are often pressured by pharmacy chains to cut costs.
- If they still refuse, ask for the pharmacy’s policy in writing. Most have one.
- If you’re still blocked, call your state’s Board of Pharmacy. They can intervene.
Some patients in Massachusetts have successfully refused substitution for Synthroid just by saying, "Per state law, I decline." No argument. No paperwork. Just a firm statement.
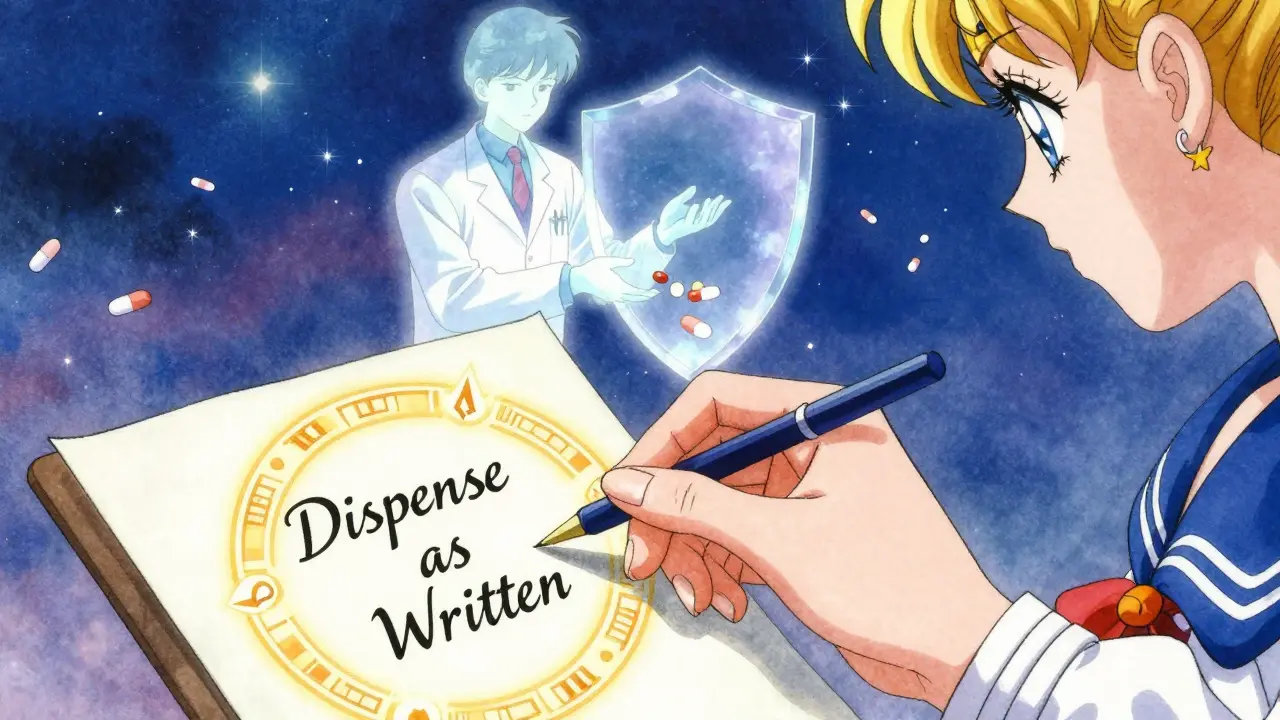
Get a "Brand Medically Necessary" Note
If you need the brand name regularly, ask your doctor to write "Dispense as Written" or "Brand Medically Necessary" on the prescription. Forty-eight states recognize this notation as a legal barrier to substitution. It doesn’t cost extra. It just takes a quick note in the prescription.Some doctors hesitate to write this because they don’t know the rules. If yours says no, show them this: the American Academy of Family Physicians supports this practice. It’s not about cost - it’s about safety.
What to Do If You’re Charged More
You might be told the brand name will cost $100 instead of $15. But here’s the twist: sometimes, paying cash for the brand is cheaper than your insurance copay for the generic. That’s because pharmacy benefit managers (PBMs) set strange pricing rules.The 2018 Know the Lowest Price Act banned "gag clauses" - rules that kept pharmacists from telling you when paying out of pocket was cheaper. Now, they’re supposed to tell you. Ask: "Is the brand cheaper if I pay cash?" If they say no, ask them to check. Many pharmacies have a price comparison tool built into their system.
GoodRx and SingleCare can also show you cash prices. You can print the coupon or show it on your phone. Sometimes, the brand name costs less than your insurance copay - even for expensive drugs.

What Happens When Things Go Wrong
In 2019, a Michigan patient had a seizure after being switched to a generic antiepileptic drug without consent. The pharmacy was sued and found liable. That case made headlines - but it’s not rare.Consumer Reports found that 28% of patients who tried to refuse substitution faced resistance. Some were told they’d lose coverage. Others were pressured into accepting a switch they didn’t want. The truth? No pharmacy can legally force you to take a drug you’ve refused - unless you’re in a state that allows automatic substitution and you didn’t say no.
If you’re harmed by an unauthorized substitution, document everything: the prescription, the generic you received, your symptoms, and any communication with the pharmacy. Report it to your state’s Board of Pharmacy and the FDA’s MedWatch program. You’re not just protecting yourself - you’re helping others avoid the same mistake.
How to Stay in Control
You don’t need to be an expert to protect yourself. Here’s what to do:- Know your state’s law. Search “[Your State] pharmacy generic substitution law.”
- Always say "I decline substitution" if you want the brand.
- Ask your doctor to write "Dispense as Written" on prescriptions you rely on.
- Check cash prices with GoodRx before letting them switch.
- Keep a log of every substitution you refuse - date, drug, pharmacy.
- If you’re switched without consent, call your state pharmacy board. They’re there to help.
Most patients only need to do this once or twice before they get the hang of it. After that, pharmacists start recognizing you. They’ll ask before switching. That’s progress.
Why This Matters
Generic drugs save the system billions. That’s good. But patients shouldn’t pay the price in health. The system was built to cut costs - not to risk safety. You’re not being difficult. You’re being smart.There’s a difference between saving money and cutting corners. You have the right to choose what goes into your body. No pharmacist, no insurance company, no pharmacy chain gets to decide that for you - unless you let them.
Next time you pick up a prescription, don’t just sign and leave. Speak up. Ask questions. Say no if you need to. Your health isn’t a cost-saving metric. It’s yours.

Amanda Eichstaedt
January 12, 2026 AT 03:13I’ve been on Synthroid for 12 years. Switched to a generic once because my insurance forced it. Within two weeks, I was exhausted, gaining weight, and my heart was racing like I’d had three espressos. I went back to the brand and felt like myself again. No doctor ever told me this could happen. Pharmacists act like it’s no big deal, but your thyroid doesn’t care about their profit margins.
Now I just say, ‘I decline substitution,’ and they nod like it’s normal. Because it should be.
People think this is about being privileged. It’s not. It’s about survival.
Alex Fortwengler
January 13, 2026 AT 01:30Of course the pharma giants want you to pay more. They own the brand names. The FDA? They’re in the pocket of Big Pharma too. Generic manufacturers are the real victims here-forced to use cheap fillers while the big boys rake in billions. And now they’re telling you to fight back? Nah. This is all a distraction. They want you to think you have control while they raise prices on everything else. Wake up.
jordan shiyangeni
January 13, 2026 AT 21:46It’s not merely a matter of preference-it’s a fundamental violation of medical integrity when a patient’s physiological equilibrium is compromised by unregulated excipients in generic formulations. The FDA’s ‘therapeutic equivalence’ designation is a statistical abstraction, not a biological guarantee. For patients on narrow therapeutic index medications, even a 2% variance in bioavailability can precipitate catastrophic clinical outcomes: seizures, arrhythmias, thyroid storm.
Pharmacists, under pressure from PBM-driven formularies, routinely disregard the Hippocratic imperative to ‘do no harm’ in favor of cost-efficiency metrics designed by corporate actuaries who have never held a stethoscope. This isn’t healthcare-it’s actuarial risk management disguised as pharmacy practice.
And yes, ‘Dispense as Written’ is legally binding in 48 states. If your prescriber refuses to write it, they are abdicating their duty. Demand it. Document it. Litigate it if necessary. Your life is not a spreadsheet.
Abner San Diego
January 14, 2026 AT 20:13Ugh, another one of these ‘you have rights’ posts. Like we don’t already know this. Meanwhile, my cousin’s kid got switched to some generic seizure med and ended up in the ER. But now you’re gonna tell me to fight the system? Good luck. The pharmacy’s gonna tell you to shut up and take the $15 pill. And if you don’t? Your insurance drops you. This isn’t about rights-it’s about who has the money to fight back.
And don’t even get me started on GoodRx. Those coupons? They’re a trap. The pharmacy gets paid less, so they start charging you extra for ‘handling.’ It’s a scam wrapped in a coupon.
Eileen Reilly
January 15, 2026 AT 16:18so like… i just asked for the brand and they were like ‘ok’?? no big deal?? i thought it was gonna be a whole thing but they just gave me my synthroid like i asked?? maybe im just lucky??
also why is everyone so dramatic about fillers?? like… its just pills. you dont even see them.
Cecelia Alta
January 16, 2026 AT 22:49Oh, here we go again. Another ‘I’m a victim of Big Pharma’ sob story. You think you’re special because your thyroid doesn’t like a different dye? Honey, I’ve been on warfarin for 17 years and switched generics six times. I’ve had zero issues. You’re not ‘sick’-you’re neurotic.
And don’t even get me started on the ‘Dispense as Written’ nonsense. That’s not a medical necessity-that’s a privilege for people who can afford to waste $80 on a pill when a $12 version works just fine for 98% of the population.
Stop turning every prescription into a drama. Your anxiety is worse than the generic.
laura manning
January 18, 2026 AT 18:20It is, unequivocally, a matter of pharmacological precision. The excipients-fillers, binders, and coatings-introduced in generic formulations may significantly alter dissolution kinetics, gastric transit time, and bioavailability profiles, particularly for drugs exhibiting narrow therapeutic indices. The FDA’s bioequivalence standards permit a 20% variance in Cmax and AUC, a threshold that is clinically indefensible for anticoagulants, antiepileptics, and endocrine agents.
Furthermore, the absence of mandatory patient consent in 24 jurisdictions constitutes a gross violation of informed consent principles enshrined in the Nuremberg Code and the Belmont Report. The commercial imperative to reduce formulary costs cannot supersede the patient’s autonomy over their physiological integrity.
It is not merely advisable to decline substitution; it is a moral imperative. One must, therefore, assert this right with unwavering clarity, document all interactions, and escalate to state pharmacy boards when obstructed. The stakes are not theoretical-they are existential.
Lawrence Jung
January 20, 2026 AT 03:01