Estradiol Level Checker
What This Means
Understanding how estradiol influences fertility and pregnancy can help women and clinicians spot problems early, plan treatment, and make lifestyle tweaks that support a healthy pregnancy.
What Is Estradiol?
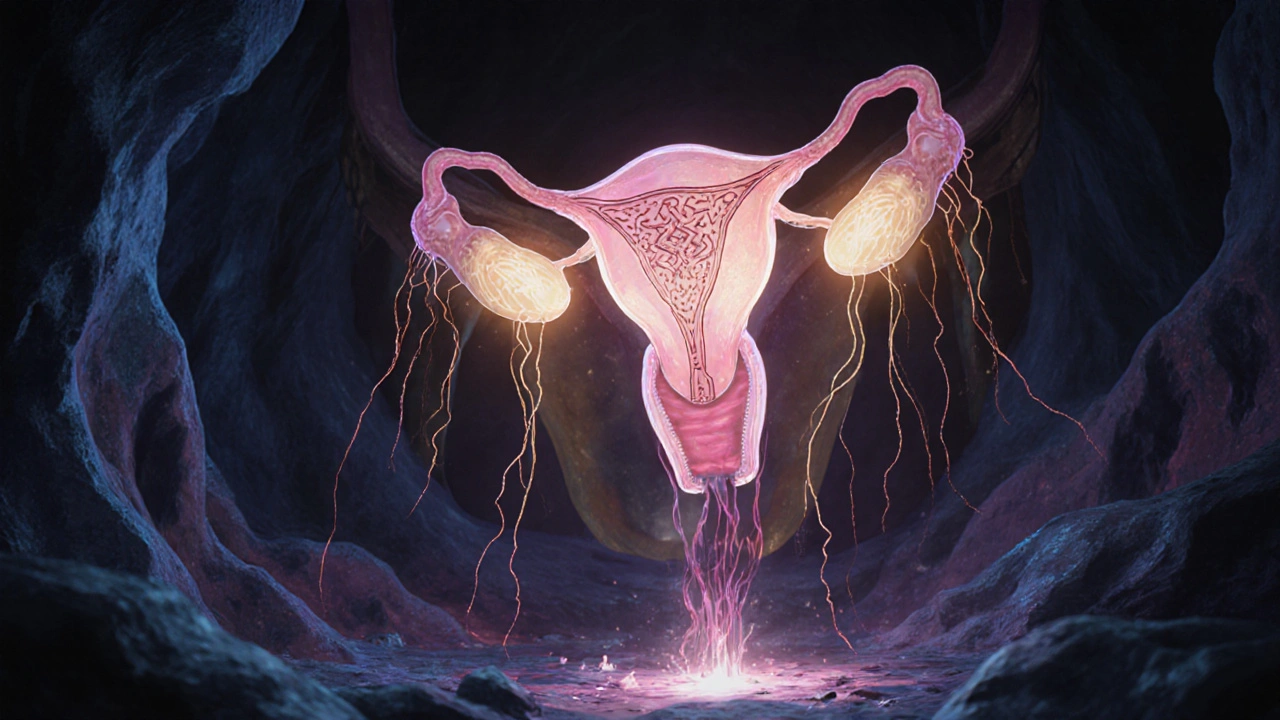
When discussing reproductive hormones, Estradiol is the most potent estrogen in the human body, primarily produced by the ovaries and, later in pregnancy, by the placenta. It belongs to the broader class of Estrogen a group of hormones that regulate sexual development and reproductive function. Estradiol binds to estrogen receptors (ERα and ERβ) in target tissues, triggering gene expression that drives growth, differentiation, and vascular changes.
How Estradiol Works in the Body
The hormone’s journey starts in the Ovaries the primary source of estradiol before pregnancy, converting androgens into estrogen via the aromatase enzyme. Once released into the bloodstream, estradiol travels bound to sex hormone‑binding globulin (SHBG) and albumin, reaching key sites such as the Endometrium the lining of the uterus that thickens each cycle to prepare for embryo implantation. During the Menstrual Cycle a roughly 28‑day sequence of hormonal events that prepares the body for potential pregnancy, estradiol levels rise and fall in a predictable pattern, coordinating follicular growth, ovulation, and luteal phase support.
Estradiol Levels Across the Menstrual Cycle
| Phase | Typical Range | Physiologic Role |
|---|---|---|
| Early Follicular | 30-100 | Initiates follicle recruitment |
| Mid‑Follicular | 100-300 | Stimulates follicle growth |
| Ovulatory Peak | 300-500 | Triggers LH surge and ovulation |
| Luteal (Post‑Ovulation) | 200-400 | Supports corpus luteum and early implantation |
| First Trimester Pregnancy | 1,000-5,000 | Produced by the placenta, maintains uterine lining |
| Second/Third Trimester | 500-1,500 | Regulates fetal growth and maternal blood flow |

Estradiol’s Role in Fertility
Three key processes rely on adequate estradiol:
- Ovulation: Rising estradiol stimulates the hypothalamus and pituitary to release luteinizing hormone (LH). A sharp LH surge then causes the dominant follicle to release its egg.
- Endometrial Preparation: Estradiol drives proliferation of the uterine lining, making it thick and vascular enough for a blastocyst to attach.
- Cervical Mucus Quality: Higher estradiol creates thin, alkaline mucus that eases sperm passage, while low levels produce thick, hostile mucus.
When estradiol stays below the optimal range, women may experience anovulatory cycles, thin endometrium, or hostile cervical mucus-all factors that lower chances of conception. Conversely, excessively high estradiol (often seen in polycystic ovary syndrome, PCOS) can disrupt the LH surge, leading to immature eggs and poor implantation rates.
Estradiol During Pregnancy
After fertilization, the developing placenta takes over estradiol production. This shift serves several purposes:
- Uterine Blood Flow: Estradiol induces vasodilation, ensuring the growing fetus receives oxygen‑rich blood.
- Fetal Organ Development: Estrogen signaling supports lung maturation, brain development, and skeletal growth.
- Maintenance of the Corpus Luteum: Early pregnancy still relies on the luteal body, which continues to secrete progesterone under estradiol’s influence.
Both insufficient and excessive estradiol levels can pose risks. Low estradiol in the first trimester is linked to miscarriage, while markedly high levels may increase the chance of preeclampsia, gestational hypertension, and abnormal fetal growth.
Clinical Implications - Testing and Managing Estradiol
Doctors typically measure serum estradiol using immunoassays or mass spectrometry. Interpretation depends on the cycle day or gestational week. In fertility clinics, estradiol monitoring guides InVitroFertilization (IVF) an assisted‑reproduction technique that often uses controlled ovarian stimulation to produce multiple eggs. Target estradiol levels help determine when eggs are mature enough for retrieval.
When levels are abnormal, several strategies exist:
- Low Estradiol: Clomiphene citrate, letrozole, or gonadotropin injections can boost ovarian estrogen production.
- High Estradiol: Adjusting medication dosages, using a “freeze‑all” approach, or prescribing aromatase inhibitors can prevent premature luteinization.
- Hormone Replacement Therapy (HRT): In menopausal women or those with hypo‑estrogenism, transdermal estradiol patches restore physiologic levels, improving bone density and sexual function.

Lifestyle Factors That Influence Estradiol
Beyond prescription drugs, everyday choices modulate estradiol:
- Body Weight: Adipose tissue expresses aromatase, converting androgens to estradiol. Women with higher BMI often have elevated baseline estradiol, which can mask ovulatory issues.
- Diet: Phytoestrogen‑rich foods (soy, flaxseed) provide weak estrogenic compounds that may subtly raise circulating estradiol, while excessive alcohol can impair hepatic metabolism, leading to higher levels.
- Exercise: Moderate aerobic activity supports balanced hormone production, but intense endurance training can suppress estradiol and cause amenorrhea.
- Environmental Exposures: BisphenolA (BPA) and other endocrine‑disrupting chemicals can mimic estrogen, confusing the body’s feedback loops and potentially altering natural estradiol peaks.
Key Takeaways
- Estradiol drives follicle growth, ovulation, and a receptive endometrium.
- Serum levels rise from ~30pg/mL in the early follicular phase to >1,000pg/mL in early pregnancy.
- Both low and high estradiol can impair conception or increase pregnancy complications.
- Testing, medication adjustments, and lifestyle tweaks are effective ways to keep estradiol within the optimal range.
Frequently Asked Questions
What estradiol level indicates ovulation?
A serum estradiol of 300-500pg/mL on day12-14 of a typical 28‑day cycle usually signals that the dominant follicle is ready for the LH surge and ovulation.
Can low estradiol cause a miscarriage?
Yes. Studies from 2023 show that first‑trimester estradiol below 1,000pg/mL correlates with a higher risk of early pregnancy loss, likely because the uterine lining isn’t sufficiently supported.
How does PCOS affect estradiol?
In PCOS, many follicles produce estrogen but the hormonal feedback is disrupted, often leading to chronically elevated estradiol that interferes with the LH surge and results in anovulatory cycles.
Is estradiol measurement reliable during IVF?
Yes. IVF clinics usually draw blood on stimulation day7-9; estradiol values guide the timing of hCG trigger and help avoid ovarian hyperstimulation.
Can diet alone normalize estradiol?
Dietary changes can modestly influence estradiol, especially when combined with weight management. However, severe imbalances often need medical therapy.
Stephen Nelson
July 14, 2025 AT 15:33Ah, estradiol, that fickle hormone that loves to make a spectacle of itself in every stage of a woman's life. One might think it simply nudges the ovaries into action, but no, it orchestrates a grand opera of cellular signaling, demanding reverence from every tissue it touches. It flirts with the endometrium, coaxing it to thicken like a well‑written sonnet, only to surrender it in a dramatic climax of menstruation. During pregnancy, it pretends to be the benevolent guardian, ensuring the placenta thrives while the fetus lounges in a sea of estrogenic bliss. Yet, ask it to keep things simple, and it throws a tantrum, spiking in the first trimester like a diva hitting a high note. Its levels are as unpredictable as a philosopher's musings on existence, rising and falling in a rhythm that would make a poet weep with envy. The medical community, bless their hearts, tries to pin it down with numbers, but estradiol laughs, reminding us that biology is not a tidy spreadsheet. Some claim that higher estradiol equals better fertility, but that is a simplistic romance that ignores the subtle dance of receptors and co‑factors. Others warn of excess, painting it as a villain that could cause complications, yet those warnings often ignore the context of individual variability. In reality, estradiol is the ultimate political figure in reproductive biology, playing both king and jester with equal flair. Its impact on implantation is akin to a master key, unlocking the uterine environment for a willing embryo, provided the timing is impeccable. It also modulates libido, mood, and even bone density, making it the Swiss army knife of the endocrine system. So, while the interactive checker on the page offers a comforting illusion of control, remember that estradiol’s true nature is to keep us guessing, ever‑alert, and forever humbled. In short, treat estradiol with the respect of a seasoned critic, yet never forget its capacity for theatrical excess.
Enjoy the ride.
Fredric Chia
July 15, 2025 AT 19:20The presented estradiol levels lack adequate statistical corroboration and should be interpreted with caution.
Hope Reader
July 16, 2025 AT 23:06Wow, thanks for the super‑clear ‘enter your value and see what it means’ tool-so intuitive, I almost felt like a lab rat 🤔 :)
Roberta Saettone
July 18, 2025 AT 02:53While the drama of estradiol is entertaining, let’s cut to the chase: during the proliferative phase, levels between 30–400 pg/mL are considered normal, and anything outside that range warrants a deeper hormonal work‑up. If you’re trying to conceive, aim for the upper end of that spectrum, but remember that timing is everything-peak estradiol should coincide with the LH surge. For pregnant patients, the expected rise is exponential, often exceeding 1000 pg/mL in the second trimester; values below that could suggest placental insufficiency. Of course, individual variation exists, so always correlate with clinical findings and ultrasound.
Bottom line: use the checker as a rough guide, not a definitive diagnosis.
Sue Berrymore
July 19, 2025 AT 06:40Great breakdown, Roberta! I’d add that staying proactive with prenatal vitamins and regular check‑ups can help smooth out those hormonal rollercoasters. Remember, you’re not alone in this journey-lean on your support network and keep that positivity flowing!
Jeffrey Lee
July 20, 2025 AT 10:26Look, I’ve read every crappy article on estradiol-its a mess. If you think a simple webpage can tell you how to manage your fertility, you’re deluded. Hormones are complex, and this tool is just a glorified calculator. Get a real doc, not this pop‑up nonsense.
Ian Parkin
July 21, 2025 AT 14:13Whilst I acknowledge the concerns expressed by my colleague, I remain optimistic that such digital tools, when employed judiciously, can serve as valuable adjuncts to clinical practice. They empower patients with immediate feedback, fostering a collaborative environment between caregiver and recipient.
With appropriate guidance, these resources may indeed enhance informed decision‑making.
Julia Odom
July 22, 2025 AT 18:00Indeed, Ian, the synergy between technology and patient education is a vibrant tapestry of hope and progress. When wielded with precision, these calculators become more than mere numbers; they transform into beacons of clarity amidst the uncertainty of reproductive health.
Marry coral
July 23, 2025 AT 21:46Look, estradiol levels are not a game. If you’re high, you could mess up your cycle. Keep it simple, track and talk to a doc.
Emer Kirk
July 25, 2025 AT 01:33i cant even deal with this hormone its like a rollercoaster and i feel sooo overwhelmed its just too much